Peritoneal Cancer Symptoms and Treatment
Peritoneal cancer, also known as peritoneal cancer, is a type of malignancy that occurs in the abdominal cavity. Symptoms are often vague and may include abdominal swelling, pain, or discomfort. Additionally, ascites, or fluid accumulation in the abdomen, is a common condition as the disease progresses. Treatment methods include hypex (hyperthermic intraperitoneal chemotherapy) and cytoreductive surgery. These treatments aim to reduce tumor size and improve the course of the disease. It is important to learn more about peritoneal cancer and consult a specialist for early diagnosis.
Basic Definition of Peritoneal Cancer
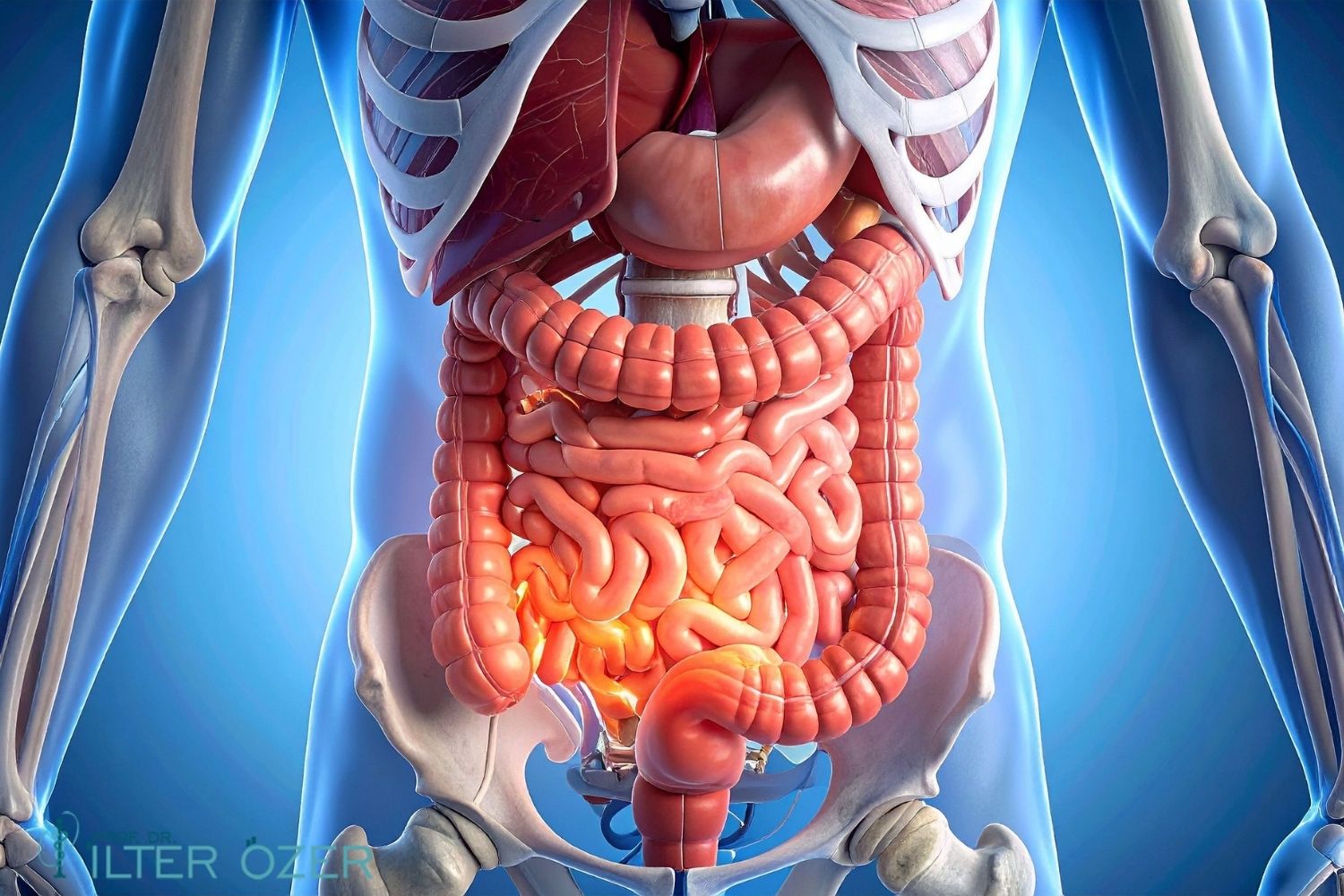
Peritoneal cancer, also known as peritoneal cancer in medical terminology, is a type of cancer in which the membrane lining the abdominal cavity (peritoneum) is affected by malignant cells. This condition usually occurs as a result of the spread of other types of cancer, but it can sometimes develop as a primary disease. Peritoneal malignancy refers to the presence of malignant cells within the peritoneum, which can significantly impact a patient's quality of life. Ascites is a condition characterized by fluid accumulation in the abdominal cavity and is a common symptom in patients with peritoneal cancer. Because this disease is usually diagnosed in advanced stages, treatment can be challenging. Treatment options include surgery, chemotherapy, and targeted therapy. Early diagnosis increases the effectiveness of treatment and prolongs patient survival. Innovative approaches such as cytoreductive surgery and HIPEC play a significant role in controlling the disease. Therefore, being knowledgeable about peritoneal cancer symptoms and conducting regular checkups are crucial.
Peritoneal Cancer Symptoms
Peritoneal cancer symptoms can vary depending on the stage of the disease and the individual's general health. Patients typically present with complaints such as abdominal discomfort, bloating, pain, and weight loss. Ascites, or fluid accumulation in the abdominal cavity, is one of the most common symptoms. Gastrointestinal problems such as loss of appetite, fatigue, nausea, and vomiting can also occur. These symptoms often worsen as the disease progresses and negatively impact patients' daily lives. When peritoneal cancer is not diagnosed in the early stages, the risk of the disease spreading and treatment options diminishing increases. Therefore, it is extremely important to seek immediate medical attention if you experience the symptoms mentioned above. Early diagnosis can significantly improve the treatment process and improve patients' quality of life. Therefore, learning about the symptoms of peritoneal cancer and having regular checkups is critical to minimizing potential risks.
Common Symptoms and Early Signs
Peritoneal cancer is a rare but serious disease, and early diagnosis can be lifesaving. This type of cancer develops in the peritoneum. Also known as peritoneal cancer, this disease often develops as a result of metastasis from other types of cancer. Symptoms are often late-noticed and can be confused with many other conditions. One of the most common symptoms is a feeling of swelling or fullness in the abdomen. This can occur as a result of fluid accumulation, called ascites. Early signs of the disease include loss of appetite, weight loss, nausea, vomiting, and abdominal pain. These symptoms often become apparent in later stages, so it's important to be vigilant. Especially in women, these symptoms can often be confused with gynecological conditions, so consulting a specialist is essential for a correct diagnosis. Early-diagnosed peritoneal cancer tends to respond better to treatment, so seeking immediate medical attention when symptoms are noticed is a critical step.
Managing Peritoneal Cancer Symptoms
Managing peritoneal cancer symptoms depends on many factors, including the patient's overall health and the stage of the cancer. A multidisciplinary approach is often adopted to alleviate symptoms. During this process, specific treatment methods may be applied to patients diagnosed with peritoneal malignancy. For example, cytoreductive surgery and HIPEC (High-Temperature Infusion Chemotherapy) are effective methods for controlling the spread of cancer. These treatment options are customized to the patient's condition and are usually administered after surgery. Various methods are also available for managing symptoms such as ascites; in this context, fluid retention and diuretic treatments can provide relief. However, because each patient's situation is unique, the treatment plan must be individually determined by the doctor. During this process, palliative care services may also be included to improve patients' quality of life. Palliative care provides support in coping with the progression of the disease while also considering the psychological and emotional needs of patients. Consequently, managing peritoneal cancer symptoms is crucial for improving patients' quality of life and facilitating the treatment process.
Imaging Methods Used in Diagnosis
Peritoneal cancer is a malignant tumor that forms in the peritoneum. Imaging techniques are one of the most important methods used in the diagnosis of this type of cancer. Imaging methods help doctors assess the extent of disease spread, the size of the tumor, and the patient's general condition. The most commonly used imaging methods include ultrasonography, computed tomography (CT), and magnetic resonance imaging (MRI). Ultrasonography is frequently used to detect fluid accumulation in the abdominal cavity (ascites) and provides rapid information. CT, on the other hand, clearly shows the tumor's size and location; It is also ideal for assessing the relationship with surrounding tissues. MRI is preferred, particularly in cases of peritoneal malignancy, because it better depicts soft tissue details. These imaging methods play a critical role in determining the stage of the disease and in treatment planning. Furthermore, the combination of these methods provides a more accurate and comprehensive assessment. Making an accurate diagnosis for patients' treatment is also crucial for improving their quality of life.
The Importance of Imaging Methods
Imaging methods play a fundamental role in the diagnosis of peritoneal cancer. These methods facilitate early detection of the disease and increase the likelihood of successful treatment. The presence of ascites, in particular, indicates that the disease may be advanced, and in this case, the source of the fluid is investigated with imaging methods. Ultrasonography not only identifies the presence of this fluid but also identifies other abnormalities in the abdominal cavity. While computed tomography provides a detailed analysis of the spread and size of tumors associated with peritoneal cancer, MRI offers a significant advantage in evaluating soft tissues. These imaging methods are also used in patient follow-up and allow for monitoring treatment response. In summary, imaging methods are critical in the diagnosis and treatment planning of peritoneal malignancy. These technologies must be used effectively to improve patients' quality of life and optimize treatment processes.
Indications for Cytoreductive Surgery and HIPEC
Peritoneal cancer, also known as peritoneal cancer in medical terminology, is a malignant tumor that usually develops in the peritoneum. If left untreated, this type of cancer can progress rapidly and significantly impact patients' quality of life. Treatment options include surgery and chemotherapy. Cytoreductive surgery and HIPEC (Hyperthermic Intraperitoneal Chemotherapy) are some of these treatment approaches. Cytoreductive surgery is a technique that involves removing tumor tissue and then injecting a warm chemotherapy solution into the abdominal cavity. This method helps destroy tumor cells and can also accelerate the patient's recovery. HIPEC, on the other hand, is a type of chemotherapy administered after surgery and targets cancer cells within the abdomen. These two methods are used effectively, especially in cases of advanced peritoneal malignancy. However, factors such as the patient's general health, tumor stage, and spread must be taken into consideration before these treatment options can be implemented. Healthcare professionals conduct a detailed assessment to develop the most appropriate treatment plan for each patient's individual situation.
Treatment Strategies for Peritoneal Cancer
The methods used in peritoneal cancer treatment vary depending on the stage of the disease and the patient's general health. Early diagnosis plays a critical role in increasing the success of treatment. Symptoms such as ascites can frequently occur as the disease progresses, negatively impacting patients' quality of life. Treatment options include surgery, chemotherapy, radiotherapy, and palliative approaches. Surgical interventions are generally performed to remove the tumor, and advanced techniques such as cytoreductive surgery may be used during this process. Chemotherapy, on the other hand, is a treatment designed to inhibit tumor cell growth and is more effective when combined with HIPEC. Radiotherapy can be helpful in destroying cancer cells. Palliative approaches aim to improve patients' quality of life and include supportive treatments such as pain management. Therefore, adopting a multidisciplinary approach to peritoneal cancer treatment is important to ensure the best outcomes for patients.
Treatment Options and Palliative Approaches
Peritoneal cancer, also commonly known as peritoneal cancer, is a malignant disease that begins in the abdominal lining, called the peritoneum. This type of cancer often spreads from other organs and is diagnosed in late stages. Various treatment options are offered for peritoneal cancer, taking into consideration many factors such as the stage of the disease, the patient's general health, and individual preferences. Surgical intervention aims to remove as much of the cancerous tissue as possible through a procedure called cytoreductive surgery. However, surgical removal of all tumors may not be possible. In these cases, additional treatment methods such as hypex (heated intraperitoneal chemotherapy) may be used. Hyperchemotherapy is a type of chemotherapy administered directly into the abdominal cavity after surgery and aims to stop the progression of the disease by targeting cancer cells. Furthermore, in cases where the disease progresses, palliative approaches become important in addition to treatment. These approaches aim to improve patients' quality of life and manage their symptoms. Services such as pain management, nutritional support, and psychological support are important components of peritoneal cancer treatment. Consequently, a multidisciplinary approach to peritoneal cancer treatment, tailoring a treatment plan to the patient's needs, is crucial.
Multidisciplinary Approach and Treatment Strategies
The collaboration of professionals from multiple specialties plays a critical role in determining the most appropriate treatment method for peritoneal cancer. Oncologists, surgeons, radiologists, and nutritionists work together throughout the patient's treatment process to develop strategies to achieve the best outcomes. For patients diagnosed with peritoneal malignancy, various imaging modalities are used at the beginning of the treatment process to assess tumor burden. These imaging modalities are crucial for understanding the extent of disease spread. Following diagnosis, cytoreductive surgery and hyperchemotherapy are the first steps in treatment planning. After surgery, additional treatment options are determined based on the patient's overall health and response to treatment. Palliative care plays a crucial role in this process, helping patients manage their symptoms and improve their quality of life. This type of care provides not only physical but also emotional and social support, helping patients and their families better manage the process. Consequently, adopting a multidisciplinary approach to peritoneal cancer treatment makes treatment more effective and improves quality of life.
Follow-up, Prognosis, and Quality of Life Management
Peritoneal cancer is a challenging process for patients and requires careful management after treatment. The progression of this type of cancer can significantly impact quality of life. Post-treatment follow-up is critical to monitoring the course of the disease and detecting potential recurrences at an early stage. Patients should attend regular check-ups with their doctor and undergo recommended imaging tests. Individuals diagnosed with peritoneal cancer or peritoneal malignancy are frequently likely to experience complications such as ascites. Therefore, it is important for patients to monitor their symptoms and contact their doctors, especially if they experience symptoms such as abdominal distension or pain. Furthermore, factors such as nutrition, physical activity, and psychological support should not be neglected to improve the quality of life after treatment. Close monitoring of patients after HIPEC can increase treatment success and positively impact their survival. The importance of family support and social network should not be overlooked in this process. Emotional support can help patients regain the motivation they lost during treatment.
Quality of Life Management and Palliative Approaches
Quality of life management plays a crucial role in peritoneal cancer treatment. In addition to methods such as cytoreductive surgery and HIPEC, palliative approaches should also be considered in the treatment process for patients with this type of cancer. Palliative care aims to improve the patient's quality of life and includes elements such as pain management, psychological support, and nutritional adjustments. Meeting the individual's emotional and physical needs is crucial at every stage of the treatment process. Especially in the later stages of the disease, patients need to establish effective communication with their families. This can provide emotional relief for both the patient and family members. Furthermore, enabling patients to make their own decisions encourages their active participation in the treatment process. A multidisciplinary approach is essential for improving quality of life; this can be achieved by a team consisting of oncologists, psychologists, dietitians, and nurses. This allows patients to receive better support throughout the treatment process and improve their quality of life.
Contact Us to Get Detailed Information About the Subject



