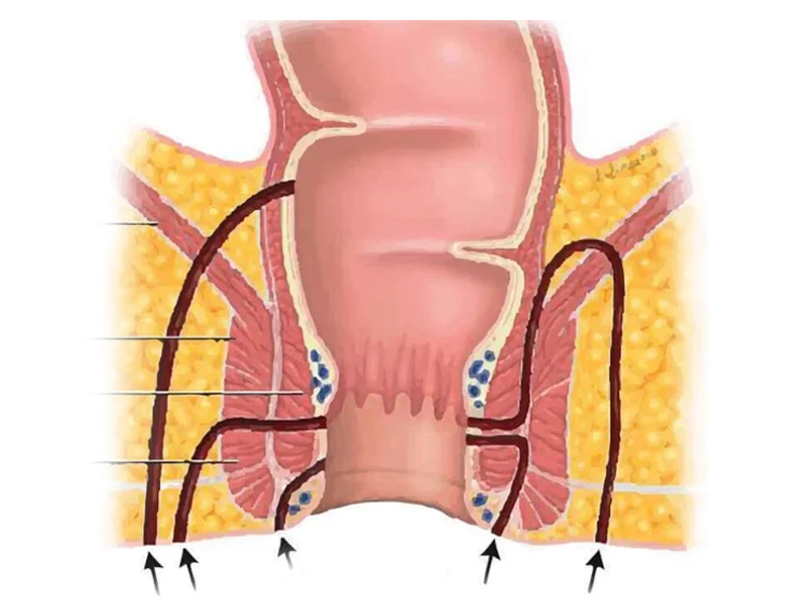
The fistula canal affects the muscle complex called the sphincter, which holds gas and feces. The internal sphincter, external sphincter and muscles in the area may be affected. The fistula tract may not be a single channel. There may be secondary channels or abscess cavities. This should be considered in treatment planning.
Anal fistulas are most commonly caused by chronic infection of the anal glands. These are called cryptoglandular fistulas. The second most common cause of anal fistulas is Crohn's Disease. Other causes include trauma, infection and tumors. The cause of the anal fistula must be taken into account in treatment planning.
Anal fistulas are most common in middle-aged men, but can also occur in women.
Classification of Anal Fistulas
1- Intersphincteric fistulas
2- Transsphincteric Fistulas
3- Suprasphincteric Fistulas
4- Extrasphincteric Fistulas
The most common fistulas are intersphincteric and transsphincteric. Intersphincteric fistulas are the most superficial and extrasphincteric fistulas are the deepest.
Fistulas can also be practically classified as simple and complicated fistulas. Simple fistulas are superficial (intersphincteric and some transsphincteric fistulas). They can be treated in a single session with an operation called fistulotomy in which the superficial side of the fistula canal (such as internal muscle, superficial external muscle) is cut and usually do not have complications such as gas and fecal incontinence afterwards. In complex fistulas, the anal sphincter muscles are significantly involved. There are higher risks of postoperative complications such as gas and fecal incontinence and recurrence. In surgical treatment, sphincter muscles should be preserved and appropriate surgical techniques should be preferred.
The following fistulas are considered complicated fistulas
- Transsphincteric fistulas involving more than 30% of the external sphincter
- Suprasphincteric fistulas
- Horseshoe fistulas
- Recurrent fistulas
- Anterior fistulas in women
- Fistulas associated with inflammatory bowel diseases
- Fistulas due to pelvic radiation (radiation therapy)
- Fistulas due to tumors
Diagnosis
Medical history and physical examination are very important in the diagnosis of anal fistula. On physical examination, it is sufficient for the diagnosis to see one or more external openings in the perianal skin with discharge. An internal hole can sometimes be detected on digital examination. Simple fistulas do not require additional imaging, but complicated fistulas require imaging before surgery. The most commonly used and most useful imaging method is magnetic resonance imaging (MRI). In addition to MRI, endoanal ultrasound (EUS) can also be used. With these methods, the course of the fistula, the presence of abscess, secondary canals and the relationship with the surrounding muscles are determined. Another method for choosing the appropriate surgical treatment is examination under anesthesia.
Treatment
Surgery is the only treatment option for anal fistulas.
In simple fistulas, fistulotomy, in which the skin side of the fistula wall and part of the sphincter muscle are cut, is the most common method. Fistulotomy is a safe operation when the correct indication is given, and gas and fecal incontinence is not seen. The recovery rate is over 95%. Correct identification of the secondary canals and the internal orifice reduces the risk of recurrence and is of critical importance. Particular attention should be paid to the presence or absence of Crohn's disease in the patients. In the presence of Crohn's Disease, the treatment plan should be changed.
In simple transsphincteric fistulas where less than 30% of the external sphincter is involved, gas and/or fecal incontinence may be observed in some patients (20%). This may be temporary or permanent. Therefore, meticulous evaluation is necessary for the choice of appropriate surgical treatment.
Fistulotomy should not be performed in the treatment of complicated anal fistulas. Sphincter sparing procedures should be performed. In complicated fistulas, the risk of recurrence of the disease and postoperative gas and fecal incontinence is higher. Today, there is no generally accepted and proven superior operation technique for the treatment of complicated anal fistula.
The most common operations for complicated anal fistulas:
- Cutting seton
- Loose seton (drainage seton)
- Fistula plugs
- Tissue adhesives
- Rectal advancement flaps
- LIFT
- TROPIS
- OTSC device
- FiLAC (laser)
- VAAFT
It is very important to choose the appropriate technique for the patient among so many surgical techniques. The complexity of the fistula, its location, presence of abscess, presence of secondary canals, etiology and the experience and preference of the surgeon are important in the choice of surgical technique.